|
Rhegmatogenous Retinal Detachment |
 |
Rhegmatogenous Retinal Detachment | ||
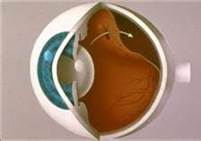
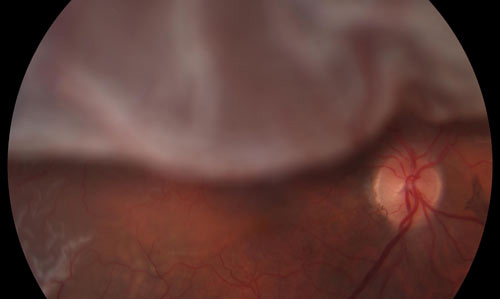
A rhegmatogenous retinal detachment is caused by a tear or break in the retina. Fluid accumulates under the retina. This separates the retina from the layer beneath, called the retinal pigment epithelium. When the retina becomes separated from the retinal pigment epithelium, you lose a portion or all of your vision in the affected eye. Because the fluid flows in and out of the break, the detachment can appear to be moving, or waving, and may change size and shape. | ||
| ||
We will all experience a separation of the vitreous as we age. This usually occurs between the ages of 50 and 70. This separation is called a vitreous detachment. This natural process usually has very few symptoms, however many persons notice an increase in floaters when this takes place. In some cases, a person may have “sticky” gel inside the eye. As the vitreous pulls away from the back wall of the eye, it may stick to the retina and cause a tear in the retina. While this process is going on, you might be seeing “flashes” of light in your field of vision. When a tear forms in the retina, the fluid inside the eye starts leaking into the tear.
The fluid pushes the retina off of its base. As the fluid under the retina increases, your vision decreases. This may happen very quickly; in a matter of hours. It can also be something that happens gradually over days or weeks. Not all tears will become a retinal detachment. It is estimated that between 4 and 18% of all persons have a retinal tear or break at some point in their life, while only 0.3% (1 in 15,000) will have a retinal detachment. |
||
| ||
You may notice you do not have as much peripheral vision in the affected eye. You may notice you have a dark area in your vision on top, bottom, or on a side of your vision. This is often described as a veil or curtain affecting your vision. Sometimes this follows an episode of flashing lights, or new floaters (dark spots). Your vision in that eye will likely be decreased, however it is possible that you may not have any noticeable symptoms if the tear is small and well into the peripheral retina. When the detachment is at the top (superior) portion of the retina, your visual symptoms will be in the lower portion of your visual field. If you have a detachment at the bottom (inferior) portion of the retina, your visual symptoms will be in the upper portion of your visual field. Additionally, when the tear is on the temporal side of the retina, your symptoms will be on the inside nasal portion of your vision and when the detachment is on the nasal side of the retina, your symptoms will be in the temporal side of your vision. The severity level of your symptoms is related to the portion of the retina that is detached. For example, if there is a small area of retina detached at the edge, you would only see a tiny area of peripheral vision impacted, or nothing at all. This would be a macula on detachment, meaning the macula has been spared so far. You would need to cover your good eye to even notice it. Conversely, if the macula or entire retina becomes detached, you will notice a significant loss of vision in the affected eye. This is a macula off detachment. Even if a retinal detachment is small and unnoticeable at the onset, the area of detachment may enlarge if more fluid seeps underneath the retina. | ||
| ||
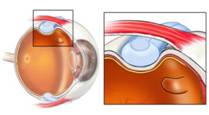
A retinal detachment is diagnosed during a dilated eye examination. An optometrist, ophthalmologist, or retina surgeon may find the retina detachment, but only a retina surgeon can repair the damage and restore your vision. A retinal detachment is diagnosed during a dilated eye examination. An optometrist, ophthalmologist, or retina
surgeon may find the retina detachment, but only a retina surgeon can repair the damage and restore your vision. A retinal detachment is usually easily identified unless it is very small. Dr. Patel will do an examination called scleral depression to locate your tear or break. A scleral depression examination allows a view of the farthest edges of the retina, where tears are most commonly found. This exam is performed in a dark room, is mildly uncomfortable, but takes just a few minutes. A small
instrument is used to apply pressure around the outside of your eye, while the doctor uses a special head set and lens to view the inside of your eye. A color photograph of the inside of your eye may be taken to document the retinal detachment. A visual field test may be performed to assess the impact to your visual field. In rare cases, a patient may present with significant vision loss because their retina has torn, and bleeding occurred from the opening. When blood mixes with the vitreous gel inside of the eye, you cannot see out of the eye, and the doctor cannot see inside the eye. In these instances, you would receive an ultrasound of the eye called a B-scan. The technology uses sound waves to image the back of the eye. This is a painless exam that allows the doctor to see if there is a tear or detachment behind the blood in the eye. | ||
| ||
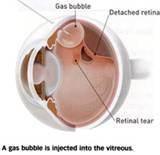
If the retinal detachment is diagnosed very early, it may be repaired with a laser treatment in a retina clinic. More advanced retinal detachments must be repaired with outpatient surgery. There are different options for surgical repair, depending on your individual circumstances. Your age, existing vision, the presence or absence of cataracts, a history of cataract or lasik surgery, and the type of tear and detachment you have all are factors that must be considered when you discuss your treatment options. The most commonly used procedure to repair a retinal detachment is the scleral buckle with pneumatic retinopexy. Scleral buckling has been used since the 1950’s and has improved with advances in technology in recent years, although the underlying principles remain the same. The scleral buckle is a silicone strip which is placed underneath the 4 extra-ocular muscles and sutured to the scleral surface between each muscle.
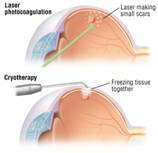
Pneumatic retinopexy was introduced in the 1980’s. In over simplified terms, it is a way of applying a band-aid to the inside of the retina. An intraocular injection of either C3F8, or SF6 gas is used to place a gas bubble inside the eye. This bubble presses on the retina, helping to seal the tear or break. In addition, either photocoagulation (laser) or cryotherapy (freezing) is used to create adhesions between the detached portion and the tissue underneath it.
While Cryopexy is an easy method of treatment for a surgeon, laser photocoagulation has advantages for you, the patient. Cryopexy is applied only to the visualized area where the detachment is. Risks associated with Cryopexy include proliferative vitreoretinopathy, cystoid macular edema, choroidal effusions, recurrent retinal detachments and macular pucker. In addition, according to The Retinal Detachment Study Group: Pneumatic retinopexy: a multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling, 13% of retinal detachments treated with cryotherapy have breaks or tears missed that require subsequent surgery to repair. It is not uncommon for retinal detachments to stem from more than 1 tear or break. Retinal Detachments are often linked to areas of thinning in the peripheral retina where breaks and tears form. Therefore the approach of 360 degree laser for the peripheral retina helps to reduce chances of additional retinal detachments and surgeries in the same eye. | ||
| ||
Some underlying eye conditions are known to have a higher incidence of retinal detachment. In many cases, a laser treatment to weak or compromised areas of the peripheral retina may reduce the risk of retinal detachment. | ||
| ||
 |
 |
|