
 |
Retinal Detachment |
 |
Retinal Detachment | ||
A Retinal Detachment is a separation of the retina from the underlying layer, called the retinal pigment epithelium. There are 3 main types: Serous Retinal Detachment, Rhegmatogenous Retinal Detachment and Tractional Retinal Detachment. The information you may have read or heard about a retinal detachment may have alarmed you. To know there is a chance of losing vision is frightening for anyone. Retinal detachment’s rarely result in a total loss of vision in the affected eye. They are most often successfully repaired with minimal vision loss. In years past, retinal detachment was thought by many to require immediate surgery or you would go blind. It is important to determine if your macula is impacted by the detachment. Commonly referred to as mac on or mac off detachments, the status of the macula prior to repair is the primary factor in determining your prognosis. While it is important to be evaluated as soon as possible after symptoms occur, it is not true that you will require surgery within 24 hours or you will go blind. One thing is true to all types of retinal detachments: you will need surgery to repair it. | ||
| ||
A retinal detachment can be caused by trauma, systemic illnesses, previous eye surgery, genetic tendencies or the aging process. The following are known factors that put you at risk for a retinal detachment: Exudative retinal detachments are uncommon. They are caused by a breakdown of cellular structure or pressure gradient. This kind of retinal detachment is usually a result of a rare congenital or systemic disorder. |
||
| ||
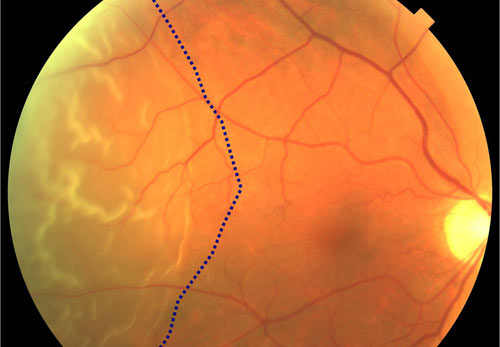
You may notice you do not have as much peripheral vision in the affected eye. You may notice you have a dark area on the top, the bottom, or on a side of your vision. This is commonly described as a veil or curtain moving across your vision. Many patients have experienced an episode of flashing lights, or new floaters (dark spots) just before the retinal detachment happened. If the detachment is at the top of your eye, this is called a superior detachment, however it will cause your vision loss to be in the lower portion of your visual field. When the lower portion of the eye is detached, this inferior defect will cause visual loss in the upper part of your visual field. The severity level of your symptoms is related to the portion of the retina that is detached. For example, if there is a small area of retina detached at the edge, you would only see a tiny area of peripheral vision impacted, or nothing at all. This would be a macula on detachment, meaning the macula has been spared so far. You would need to cover your good eye to even notice it. Conversely, if the macula or entire retina becomes detached, you will notice a significant loss of vision in the affected eye. This is a macula off detachment. Even if a retinal detachment is small and unnoticeable at the onset, the area of detachment may enlarge if more fluid seeps underneath the retina. | ||
| ||
A retinal detachment is diagnosed during a dilated eye examination. An optometrist, ophthalmologist, or retina surgeon may find the retina detachment, but only a retina surgeon can repair the damage and restore your vision. In rare cases, a patient may present with significant vision loss because their retina has torn, and bleeding occurred from the opening. When blood mixes with the vitreous gel inside of the eye, you cannot see out of the eye, and the doctor cannot see inside the eye. In these instances, you would receive an ultrasound of the eye called a B-scan. The technology uses sound waves to image the back of the eye. This is a painless exam that allows the doctor to see if there is a tear or detachment behind the blood in the eye. | ||
| ||
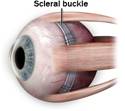
When a minimal retinal detachment is diagnosed very early, it may be possible to repair it with a laser treatment in our office. More advanced retinal detachments must be repaired with outpatient surgery. Several different surgical options exist for the repair of a retinal detachment. Your surgery will be tailored to address your specific needs. For instance, if you have already had cataract surgery in the past, a vitrectomy with scleral buckling may be the best option for you. If you have never had cataract surgery, or are a young adult at the time of your detachment, it might be
preferable to place a scleral buckle without doing a vitrectomy. A vitrectomy will cause a cataract to form postoperatively. If you have had cataract surgery, you cannot get another cataract. A scleral buckle is a silicone band that is placed underneath the extraocular muscles, and sutured in place.
A common procedure included in any type of retinal detachment surgery is the placement of a gas bubble. The SF6 gas bubble is short acting, and will be in place for a few weeks. The C3F8 gas bubble is longer acting, and will be in place for 8-12 weeks. The length of time the bubble stays in the eye is dependent on the body’s ability to metabolize or absorb the bubble according to chemical formulas. The gas bubble is a critical part in keeping the retina in place during reattachment. These gases are lighter than water, and will rise to the top of a fluid filled container. Therefore, when you sit up straight and look forward, the gas bubble is at the top of your eye. The retina is on the back wall of the eye, so to make the bubble apply pressure to the retina, your face must be positioned parallel to the floor.
Special chairs are available for rent to help you maintain the proper positioning. The first week after surgery is the most restrictive. Your ability to maintain a face down position will impact the quality of vision you have postoperatively.
While this is a difficult time for our patients, most are able to regain nearly the same level of vision they had prior to the retinal detachment. It is rare that anyone goes blind in the eye that suffers a detachment. | ||
| ||
Some underlying eye conditions are known to have a higher incidence of retinal detachment. In many cases, a laser treatment to weak or compromised areas of the peripheral retina may reduce the risk of retinal detachment. Safety glasses and goggles help prevent trauma to the eye that can cause retinal detachment. A healthy lifestyle and careful management of diabetes also helps to reduce your risks. | ||
| ||
 |
 |
|

 -
-
