
 |
Diabetic Retinopathy |
 |
Diabetic Retinopathy |
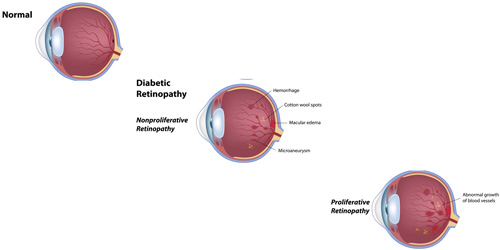
If you have diabetes, diabetic retinopathy is nearly an eventual certainty after 10 years, even if the diabetes is well controlled. On rare occasions, patients do not have any impact on the retina, however, this is not common. Diabetic retinopathy is categorized into two groups: Non-proliferative, and proliferative. Both are characterized by vascular complications in the retina. This is the leading cause of blindness in the United States for persons 20-65 years old. Occassionally in our clinic, a retinal examination because of vision problems is the first time the patient becomes aware they have diabetes. |
|
Diabetes mellitus. |
|
You may not have any vision problems in the early stages of diabetic retinopathy, so it is important to have regular retinal examinations to maintain your sight. Retinal inflammation from diabetes may cause distorted or blurry vision. Bleeding from diabetic retinopathy may cause cloudy vision. If the bleeding is severe, it may cause a loss of vision in the eye affected. |
|
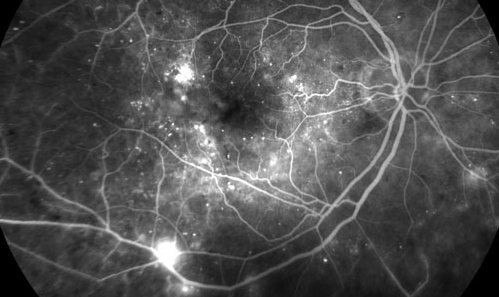
Diabetic retinopathy is diagnosed by retinal examination, special pictures called a fluorescein angiogram, an OCT (optical coherence tomography) scan and sometimes an ultrasound of the eye. |
|
Mild diabetic retinopathy may not require any treatment. Moderate to severe diabetic retinopathy may require injections of medication to the eye, laser treatments in the retina, or in some cases surgery. |
|
Maintaining a Hemoglobin A1C level of 7.0 or below will help prevent diabetic retinopathy from advancing to severe stages. Having regular retina examinations and any necessary treatments will help maintain your vision once diabetes has impacted your eyesight. |
|
 |
 |
|
