
 |
Macular Pucker |
 |
Macular Pucker | ||
Your macula is a small area in the center of your retina. While this area is small, it has a big impact on your vision. The macula allows you to see fine details clearly. A healthy, normal macula should lie flat against the back wall of the eye, allowing a smooth surface for light rays to reflect off of. A smooth flat macula, allows crisp, sharp fine details for seeing things like small print. A macular pucker is a layer of tissue that forms on the surface of the retina. The macular pucker causes contraction of the retina so that it becomes wrinkled in appearance. You may have heard this referred to as an epiretinal membrane or a wrinkle on your retina. | ||
| ||
Not everyone gets a macular pucker. However, it’s most common cause is the ageing process. As you age, the vitreous gel that fills the inside of your eye slowly shrinks back away from your retina. During this time, the gel separates from the retina. As the gel is separating, tiny cells called hyalocytes may fall to the surface of the retina. Sometimes these cells proliferate along the innermost layer of the retina, near the macula. It is believed that in some cases, the macular pucker may be caused by glial cells that proliferate after escaping an abnormal defect in the retina’s internal limiting membrane layer. Either way, it is an age related issue that results in an abnormal layer growing on the surface of your retina. With time, this layer causes your retina to become pulled out of shape. It has the effect of scar tissue, pulling and tightening the retina, sometimes twisting it. If you have had a trauma to the eye, or you have an existing retinal disorder, you may be more susceptible to a macular pucker. Retina conditions that are associated with macular puckers include a detached retina, a tear in your retina, retinal inflammation, and disorders of the vascular structure in your eye. |
||
| ||
When a macular pucker is forming, you may notice central vision which is blurred, distorted or have a gray spot, or you may experience difficulty seeing fine detail and reading. You might notice it is becoming difficult to enjoy your favorite hobby or sport because you are not seeing as well. Maybe you need to read labels in the grocery store, and it is taking longer to study the writing on them. It could be that you notice the boxes on a crossword puzzle don’t look square anymore. It is however, possible you may have a macular pucker growing for months or even years before noticing the symptoms. Often a patient comes to our office with the complaint that it’s progressively getting harder for them to read. One of the first things we do is to have you cover one eye at a time and read. Surprisingly, many of you do not try this at home, and are unaware that the problem is only in one eye. Consequently, some of you will arrive in our clinic only after an annual dilated eye exam where the doctor was unable to correct vision in one of your eyes with a new lens. Unlike cataracts and presbyopia, macular puckers most commonly impact only one eye, or one eye much more than the other. | ||
| ||
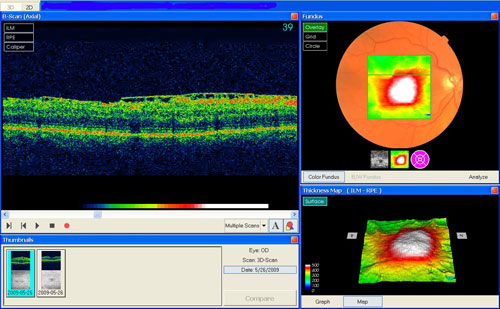
A full comprehensive eye exam is required to detect a Macular Pucker. A complete medical history and special pictures will be obtained. While the slit lamp examination with a contact lens gives the doctor the best view of your macular pucker, the photographs and scans provide important information on how to manage your treatment. A fluorescein angiogram uses dye that is injected into a vein in your arm, and a special retina camera. Photographs are taken before the dye is injected, while the dye is entering the vessels and after it has completely circulated. The dye takes only seconds to reach the vessels in your eyes. The dye will highlight areas of abnormality in the retina. Macular puckers may cause many structural changes like tortuous vessels, macular edema, or vascular leakage caused by retinal traction. These are readily apparent on fluorescein photographs, but may have been difficult to see or invisible during the slit lamp exam. The angiogram will also reveal any additional underlying retinal pathology that may impact the way your macular pucker is treated. An OCT scan is a quick and easy way to document the progress of your macular pucker both preoperatively and postoperatively. This scan shows the layer where the retina and the vitreous meet. In a normal retina, there should be a dip in the scan at the place where your macula is. In a scan where a macular pucker is growing, the scan may be straight across, or even elevated. The scan will reveal if your vitreous has not cleanly separated from your retina and is causing traction on your macula. Traction may lead to a macular hole or pseudohole or lamellar hole. The OCT scan will also reveal the thickness of the abnormal area where the macular pucker is pulling the retina out of shape. This is called retinal thickening. When retinal thickening occurs, it is directly related to the amount of distortion you experience in your near vision. The thickness of your retina is measured in microns. Normal thickness is around 250 microns. | ||
| ||
For mild symptoms no treatment may be necessary, however, if you develop an increase in symptoms and are bothered by these surgical intervention may be needed. In the earliest stages, if you maintain good vision by keeping your lens prescription current, you and your doctor will probably agree to simply observe and document the macular pucker. When symptoms progress to the point that you experience a negative impact on your normal activities, you and your doctor may discuss the best time and approach for a surgical intervention. The surgery is called a vitrectomy and is done as an outpatient procedure. Dr. Patel currently uses the newest equipment and surgical techniques available to reduce your risk factors and maximize your visual
outcome. Statistically, there is a 5% chance of reoccurrence when a macular pucker is surgically removed. This has been significantly reduced using Dr. Patel’s techniques. The surgery requires 3 tiny incisions, and is performed under a microscope. The healing from the surgical procedure itself takes a minimum of 6 weeks. In the first days following surgery, your vision may be worse than before surgery. The healing occurs very gradually. You do not suddenly have better vision as patients who have cataract surgery do. About 90% of the healing takes place
in the first 6 weeks, and the remaining 10% takes up to 6 months or more. You are able to resume your normal activities within a few days of surgery. The goal after the macular pucker has been removed is to encourage the retina to become as flat as possible. With this in mind, the doctor may place an air bubble or a short acting gas bubble in your eye during surgery. When a bubble is placed to help flatten your retina, you will be asked to do some special positioning during the first few days of your recovery. Your vision may not ever improve to what you had prior to the macular pucker, but most often it improves at least a line on the vision chart over time. The level of improvement in your distortion depends on the flatness of your retina after healing. Your vision will stabilize so there is no further loss from this condition. If you have never had cataract surgery, you should expect a cataract to form postoperatively that will need to be removed at some point in the future. If you have already had a cataract removed, you cannot develop another one. | ||
| ||
A healthy lifestyle and regular eye examinations are important in the prevention and early detection of a macular pucker. | ||
| ||
 |
 |
|
